Recapping the Berman Institute at ASBH 2020

The Berman Institute will be well represented at the 22nd annual meeting of the American Society for Bioethics and Humanities (ASBH), with a group of faculty, fellows, and students scheduled to present online.
View the full schedule and summaries of all Berman Institute presentations.
 |
You can also follow us on Twitter: #ASBH19, featuring our @bermaninstitute, @aregenberg, @kahnethx, @tnrethx, @DiStefano_MJ, and more. |
Special Events

Plenary: Social Justice and Bioethics through the Lens of the Story of Henrietta Lacks
October 15, 2020
1:15-2:30 p.m.
Join Jeff Kahn, Ruth Faden, Jeri Lacks (granddaughter of Henrietta Lacks), and Patricia King for a panel discussion examining social justice and bioethics through the lens of issues and challenges raised by the story of Henrietta Lacks and the HeLa cell line derived from her cells.
Antigone in Ferguson: Free Online Zoom Performance
October 17, 2020
6- 8:30 p.m.
A groundbreaking project that fuses dramatic readings by acclaimed actors of Sophocles’ Antigone with live choral music culminating in a powerful, healing discussion that will foreground the perspectives of people in Baltimore whose lives have been impacted by racialized police violence and health inequity
Overview: Ethical Concerns in Responding to Coronavirus
For comprehensive Covid-19 Ethics and Policy Resources, visit our dedicated webpage, bioethics.jhu.edu/coronavirus.
The ongoing coronavirus outbreak vividly demonstrates the important role of bioethicists in leading the charge for equitable and effective public health policies.
“Through years of experience and scholarship, and tested through multiple threatened and actual epidemics, there now exists a rough consensus about the ethical principles that should guide responses to this latest threat,” said Jeffrey Kahn, Andreas C. Dracopoulos Director of the Berman Institute of Bioethics. “Bioethicists from the Berman Institute have been leaders in shaping this framework.”
The Berman Institute is working to disseminate these ideas through social media, appearances in traditional news media, and through other means, as widely as possible on an ever-expanding range of issues, including:
Human Research
“For reasons of safety, efficacy, and ethics, it’s usually better to test vaccines on animals before humans. You have to have good reason to say, ‘We need to go straight to humans or go to humans at this particular point.'”
“Kahn worries about people signing up to be in the trial because they think the vaccine could give them immunity before it becomes available to everyone else. In reality, this kind of early trial is just to make sure that the vaccine is not toxic and does indeed provoke some kind of immune response in people. Participants are very unlikely to be fully immunized to the virus over the course of their participation.”
- Jeff Kahn, The New Republic (March 16)
Travel Restrictions
“A critical principle in outbreak response is that governments should implement the least restrictive measure that can still achieve the public health objective. The goal is to balance the freedom of individuals against the restrictions on freedom required to achieve legitimate protections of the public’s health, with public and transparent justification of policy decisions. Quarantine is considered a measure of last resort given the severe restrictions it imposes on individual liberty.”
- Jeff Kahn, Global Health Now and NPR Baltimore
Inequitable Impact of School Closings
“As in all public health emergencies, poor children and poor families will suffer the most. An ethically defensible policy of school closures needs not only to meet the bar of public health necessity. Government agencies and community organizations in education, nutrition assistance and housing, as well as public health, must also be planning to take active measures to mitigate the disproportionate burden that will fall on our most vulnerable children.”
- Ruth Faden, founder of the Berman Institute and Philip Franklin Wagley Professor of Biomedical Ethics, Education Week and The Baltimore Sun
Dr. Faden’s prescient Education Week piece helped prompt discussion among K-12 educators nationwide. Officials in numerous states have sought USDA waivers that will enable them to continue providing free meals during school closures.
Allocation of Scarce Resources
“It is appropriate and accurate to reassure the public that most people who contract Covid-19 will recover fully on their own. At the same time, the public needs to be prepared for the possibility of more dire scenarios. Participants in our study were adamant that politicians, and health officials, be transparent and honest about the prospect of and plans for the rationing of ventilators and other equipment. In health emergencies, experts often ask the public to heed the advice of public health professionals; in the case of planning for situations involving scarcity, it is equally important that the experts heed the advice of the public.”
- Faden and Alan Regenberg, Washington Post
Inequitable Impact of Social Distancing
“The implications of some of these public health measures are so wildly different for people who are differently situated in the United States that the social distancing [decision] is not our only decision. It’s our first one, and then there’s a very different set of ethical dominos that follow from that.”
- Nancy Kass, STAT News
Kass listed a number of ethical considerations she’s concerned about, like making sure there’s adequate income replacement for workers unable to earn a living, making sure grocery stores stay open and accessible, and even making sure people have access to the creature comforts that make social distancing bearable.
Inequity of Work Requirements During Pandemic
“Income replacement for people whose employment has been curtailed by the government isn’t just an economic issue, it’s an ethical one. Likewise, we need to consider what to do for workers in jobs where sufficient protection from infection cannot be provided. While we have expectations of certain healthcare professionals, like doctors and nurses, who have taken oaths to continue working even when it puts them at personal risk, the same isn’t true for hospital support staff or grocery store checkers. We can’t simply expect those workers to continue facing risks that others can avoid.”
- Kahn, with Kass, Public Health on Call (Bloomberg School of Public Health podcast)
Equity in Vaccine Development
“Historically, the interests of pregnant women have not been adequately included in global responses to outbreaks and epidemics. As the world rushes to develop new vaccines against Covid-19, we must ensure that, this time, pregnant women and their babies will not be left behind. Developing a coronavirus vaccine that they are unable to use would be not only a tragedy but a grave injustice.
- Faden and Carleigh Krubiner, STAT News and The Boston Globe
The article was included as required reading for the 38th Annual Congressional Leadership Conference of the American College of Obstetricians and Gynecologists, as physicians came to Washington from across the country to meet legislators and help shape public policy. Faden and Krubiner’s co-author of the STAT and Boston Globe article and collaborator in the PREVENT project, Ruth Karron of the Johns Hopkins Vaccine Initiative, was quoted in a March 3 New York Times article, “What Pregnant Women Should Know About Coronavirus.”
Patient Privacy and Contact Tracing
“Doctors don’t out people. Whether it’s HIV, syphilis, coronavirus or anything else, people simply won’t show up to their doctor if they feel they might be outed for a condition.”
- Kahn, USA Today and NPR Philadelphia
Impact on Incarcerated Individuals
Detention and correctional spaces are the “perfect environment for the spread of COVID-19. So when we talk about social distancing, it’s almost impossible in prisons unless you have complete lockdown – basically, put everybody in solitary confinement.”
- Len Rubenstein, Axios
The Berman Institute continue to offer insights and expertise to aid in the response to the monumental challenges posed by the outbreak.
Related Berman Institute Resources
- 2019 Robert H. Levi Symposium: “Containment: Exploring the History, Politics and Ethics of Infectious Disease Response in a Post-Genomic World”
This symposium brought together experts to explore the shifting politics of containment from the nineteenth century through the Cold War to the present, to inform best practices for infectious disease preparedness and response from the local to the global scale. - Ethics Guidance for the Public Health Containment of Serious Infectious Disease Outbreaks in Low Income Settings: Lessons from Ebola
In 2019, the Berman Institute and partners published a report and other resources, as products from a project to provide an ethics guidance document for public health professionals to use in infectious disease outbreak response. The guidance makes clear that regardless of geography, infectious disease outbreak response strategies should be effective, fair, respectful and transparent. - The Bellagio Meeting on Social Justice and Influenza
In 2006, Dr. Faden was among a group of 24 experts in public health, animal health, virology, medicine, public policy, bioethics, law and human rights from 11 countries that met to consider questions of social justice and the threat of avian and human pandemic influenza. The consensus of the group was that efforts to prepare for and respond to a pandemic should take account of the needs and interests of the disadvantaged.
Developing a Better Understanding of Public Private Partnerships for Nutrition: Towards the Next Generation of PPP Models
The Food Systems Dashboard
Join the Berman Institute at ASBH 2019

The Berman Institute will be well represented at the 21st annual meeting of the American Society for Bioethics and Humanities (ASBH), as a group of faculty, fellows, and students are headed to Pittsburgh, PA, October 24 – 27, 2019.
Preview our diverse presentations (full program available online), and plan a visit to our booth in the ASBH exhibit hall replete with BI swag – (including this year’s limited edition wood cube basil planter!)
 |
You can also follow us on Twitter: #ASBH19, featuring our @bermaninstitute, @aregenberg, @kahnethx, @tnrethx, @DiStefano_MJ, and more. |
|
SPECIAL EVENTS:Thursday, Oct. 24, 7:30 pm-9:30pm: Book Release Party – Celebrating recent Oxford University Press Books published by Berman Institute Faculty. Friday, Oct. 25, 6:00 pm-8:00 pm: Reception – hosted by the Johns Hopkins Berman Institute and the Wellcome Trust.
|
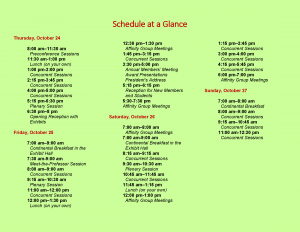
Full Schedule:
–Thursday, October 24–
Concurrent Sessions – 1:00 pm–2:00 pm | Location: Room 303
Improving Informed Consent in Research
Joseph Ali, JD; Holly Taylor, PhD; Nae-Yuh Wang, PhD; Daphne Washington, BA

Informed consent documents remain too long, complex and legalistic, threatening the ability of even committed potential research participants to understand research. Recent changes to U.S. regulations (Common Rule), as well as significant bioethics literature, suggest consent forms should be shorter and simpler. Despite decades of consent research, there is no simple, adaptable, evidence-based approach to improving participant understanding of research. Robust study of consent interventions in diverse, non-simulated research settings is critically important to effective communication of research information and adaptation of new (presently vague) consent “key information” requirements. In this session, we present the methods and core findings from a Greenwall Foundation-funded three-arm randomized consent intervention study conducted at a large research-intensive institution. This study developed and tested two reproducible consent approaches that are concise, emphasize key information, provide information in discrete chunks, and use lay language. Individuals considering enrollment across five ongoing clinical studies (target n = 300 participants) were randomized to receive either 1) the standard consent form and process (control), 2) a briefer consent fact sheet, or 3) a video consent summary based on the fact sheet and consisting of a conversation between the study PI and an actor playing a potential participant. A previously developed tool (Consent Understanding Evaluation) was modified to measure both consent understanding and satisfaction. Data collection will be complete by April 2019. Analysis will be complete by June, with methods and key findings ready to share for October.
1:00 pm-2:00 pm | Location: Room 304-305
The Ethics of Harm Research with Nonhuman Animals
Anne Barnhill, PhD, Jake Earl, PhD, David Wendler, PhD

Over the past several decades, conversation and collaboration among bioethicists, scientists, and policy makers have led to substantial improvements in the well-being of nonhuman animal subjects in biomedical research. While this progress is commendable, there are no regulations that limit the nature or amount of harm that researchers may impose on nonhuman animal subjects. Should there be any limits on the sorts of harm that nonhuman animal subjects suffer, and if so, what should those limits be? Each of the three panelists offers a distinctive perspective on the justifiability of imposing serious harms on nonhuman animal subjects, which together have significant ethical and policy implications for the conduct of biomedical research. The first panelist will set the stage by surveying the ethical issues raised by infection challenge trials with nonhuman primates. These studies are an excellent test case in that they impose serious harms on cognitively sophisticated animals while providing invaluable information for fighting disease in humans. The second panelist will argue that there are no harms that in principle cannot permissibly be imposed on most nonhuman animals, including most nonhuman primates. This is because unlike most humans, most nonhuman animals can be fully compensated for any harms they might suffer in research. The third panelist will argue that there are some harmful experiences that are so intrinsically bad that they cannot be fully compensated, and therefore the permissibility of harming nonhuman animal subjects in biomedical research will depend on answers to difficult questions about the nature and value of suffering.
1:00 pm – 2:00 pm | Location: Room 321
Disparities in Access to Fertility Care in the United States: Ethical Considerations for Equitable Solutions

There are significant disparities in access to fertility services in the United States. These disparities exist along lines of race, ethnicity, education, income, geographic location, marital status, gender identity, sexual orientation and comorbid conditions (e.g., HIV, Hepatitis C). In this paper, I will argue that these inequalities represent injustices and therefore demand rectification. The disparities in access to care exist for certain groups with shared characteristics and these groups are overall socially and historically disadvantaged.
However, proposed solutions will also raise ethical issues that require careful consideration. For example, passing a policy that mandates insurance coverage of in vitro fertilization raises questions about eligibility, resource allocation, distributive justice and limitations on which reproductive technologies ought to be covered. Such a policy also fails to address barriers other than cost, such as geographic location, which may perpetuate existing disparities. Given that barriers to care include financial, geographical, and sociocultural factors, I will argue for the necessity of multifaceted solutions. Ultimately, my investigation reveals that proposed solutions to reduce disparities in access to fertility care raise ethical issues of their own. These issues are not reasons for inaction, but rather ought to be carefully considered when evaluating policy solutions. I will conclude with recommendations for mitigating ethical concerns that arise from policies that aim to address disparities in access to fertility care in the United States.
2:15 pm-3:45 pm | Location: Room 317-318
The Hastings Center 2019 Henry Beecher Award Session

Ruth Faden, PhD, MPH, Philip Franklin Wagley Professor of Bioethics, Johns Hopkins University is the 2019 recipient of The Beecher Award for Lifetime Achievement, which is The Hastings Center’s most prestigious award for life time achievement. Founder of the Johns Hopkins Berman Institute of Bioethics, Dr. Faden’s work has profoundly influenced innumerable aspects of our field and, perhaps more importantly, helped to shape public policy on some of the nation’s most pressing issues: from HIV testing of pregnant women to food and agriculture policy, and many aspects of science policy, including stem cell and embryo research. She has also powerfully critiqued the prevailing research ethics paradigm in the United States, encouraging major shifts in how we think about the oversight of comparative effectiveness research. In 1994-5, she chaired the United States Advisory Committee on Human Radiation Experiments, which issued a report President Bill Clinton said “should be engraved in our national memory.” In her latest book, Structural Injustice: Power, Advantage, and Human Rights (September 2019, Oxford University Press), Dr. Faden and co-author Madison Powers build on their longstanding call for bioethics to expand its understanding of justice to put forward a groundbreaking theory of social injustice, more broadly. Their theory forges links between human rights and fairness norms and is built to fit a real-world characterized by deprivation, human rights violations, disadvantage, and unfair power relations, both within and across nations. This session will also include presentation of the inaugural David Roscoe Early Career Essay Award. Through this award, which includes a $2,000 prize, The Hastings Center aims to identify and celebrate early-career post-docs and junior faculty for excellence in a published paper that has brought fresh analysis to the social and ethical implications of advances in science and technology. This year’s award winner will be named for the first time at this event. The session will include introductory comments by Mildred Solomon, president of The Hastings Center, who will then interview Professor Faden, in a wide-ranging discussion of her reflections on her career, the major issues she has addressed, and where she would like to see the field going in the future. David Roscoe, the former long-time chair of The Hastings Center, and now chair of its Advisory Committee, will present the Roscoe Essay Award and its recipient will make brief remarks. There will be plenty of time for questions from the audience.
2:15 pm-3:45 pm | Location: Room 310-311
Integrating Procedural and Substantive Values to Assess the Ethics of Process in the Healthcare Priority Setting

High quality universal health coverage is an increasingly important policy objective for many countries, especially low- and middle-income countries. While health care demand may be infinite, resources for health are finite. Health care priority-setting is thus inescapable, leaving countries with difficult choices regarding what services will be covered by publicly funded health systems. In discussions of the ethics of health care priority-setting, two questions dominate: 1) what substantive criteria ought to inform priority-setting decisions, and 2) what processes ought to guide priority-setting? These questions are typically explored independently. For instance, Accountability for Reasonableness – the dominant account of process – was developed to achieve fair and legitimate priority-setting decisions independent of the substantive criteria chosen to inform those decisions. I defend a novel approach for assessing the ethics of process in health care priority-setting that integrates procedural and substantive ethics considerations to address key critiques of and expand on Accountability for Reasonableness. I show how this novel approach provides better guidance for adapting to specific national contexts and gives much needed attention to values beyond fairness and legitimacy. I also discuss novel benefits of pursuing parallel and mutually coherent – rather than independent – substantive and procedural ethics frameworks for health care priority-setting. First, substantive values beyond fairness such as respect and solidarity may provide additional or stronger justification for the selection and design of process elements. Second, process elements may help decision-makers properly apply a substantive value – such as equity – when assessing an intervention for coverage.
4:00 pm-5:00 pm | Location: Room 302
A Drama of Resilience and Remembrance: Reflecting on Life, Loss, and Liminality
Lynn Bush PhD, MS, MA, Bob Truog MD, MA, Christine Mitchell RN, MS, MTS, FAAN, Cheryl Lew, MD, MSEd, MSBioethics, FAAP, Karen Rothenberg, JD, MPA, Ben Wilfond, MD

In remembrance of the Tree of Life tragedy our host city experienced and the extraordinary resilience demonstrated in the aftermath of such trauma and loss, a new dramatic vignette-play provides a stage for the ASBH community to explore the conference’s thematic concepts in the symbolic context of a vastly different “tree of life” scenario. Set in a pediatric hospital, the drama spotlights life, loss, and liminality surrounding some ethically controversial cutting-edge technologies for which Pittsburgh and the geographically diverse panelists’/actors’ medical centers are among the field’s leaders, including regenerative and gene therapies for rare diseases as well as “elective” organ transplantation to improve quality of life and experimental fetal therapies. Utilizing dramatic narrative-vignette pedagogy, the twenty minute play stimulates interprofessional dialogue among ASBH bioethics and humanities-scholars about ethical dilemmas and psychosocial challenges raised by the characters. The session will critically examine complex issues facing our multicultural society as we implement these technologies and address concepts of normalcy and illness; decision-making evoking hope and grief; along with concerns about health disparities, justice, and equity in access to limited resources, including consideration for the disability community. Following the play, panelists (PhD; RN; MDs; all experienced in creative educational approaches) will present their varying perspectives, and actively engage the actors and audience in 40 minutes of robust discussion reflecting on the ethical justifications and policy implications of therapeutic boundaries when the individuals are vulnerable, the resources are limited, the disorders are rare, the evidence is not clear, and the treatments are not trivial. [Actor-panelists include: Lynn Bush, Bob Truog, Christine Mitchell, Cheryl Lew, Karen Rothenberg, Ben Wilfond].
4:00 pm-5:00 pm | Location: Room 316


4:00 pm-5:00 pm | Location: Room 303

7:30 pm-9:30 pm | Location: The Westin Pittsburgh, Butler Room
Book Release Party
The Johns Hopkins Berman Institute of Bioethics invites you to a Book Release Party (dinner will be served) celebrating recent Oxford University Press books by Berman Institute Faculty:
Beyond Consent (2nd Edition)
Jeffrey P. Kahn, Anna C. Mastroianni, and Jeremy Sugarman, eds.
Structural Injustice: Power, Advantage, and Human Rights
Madison Powers and Ruth Faden
The Oxford Handbook of Public Health Ethics
Anna C. Mastroianni, Jeffrey P. Kahn, and Nancy Kass, eds.
–Friday, October 25–
Concurrent Sessions – 8:00 – 9:00 am | Location: Room 306-307
“Because It’s My Child and I Want to Know”: A Survey of Pregnant Women’s Views on the Utility of Ultrasound Screening for Fetal Anomalies
Margot Kelly-Hedrick, MBE, Marielle S. Gross, MD, MBE


Screening ultrasounds are routinely performed during pregnancy, primarily to diagnose major fetal anomalies that may influence women’s decision to have an abortion. As ultrasounds have grown more sophisticated, women are also receiving more detailed findings with variable clinical significance. Meanwhile, some women undergoing screening ultrasounds may not consider abortion regardless of findings, whereas others may find their access to abortion increasingly limited. Little is known about how women view the utility of prenatal anomaly screens.
We surveyed 286 pregnant women immediately before scheduled ultrasounds at an academic tertiary care center. Quantitative and qualitative questions explored views surrounding ultrasound results and abortion for fetal anomalies. Almost all women wanted to know if there were abnormal ultrasound findings; thematic analysis of reasons included being prepared, valuing awareness, and the importance of results for clinical decision-making. Women reported both general (e.g., baby’s health) and specific worries (e.g., Down syndrome) about the upcoming test. About half would consider abortion for anomalies; most focused on fetal prognosis and a minority discussed maternal considerations. Those who would not consider an abortion were most likely to cite personal or religious reasons. In this population, white women were significantly more likely than black women to consider an abortion for fetal anomalies.
These findings highlight women’s perceptions of prenatal ultrasounds not only as informing clinical decision-making – either for abortion or interventions for fetal benefit – but also as an inherently valuable source of information and preparedness. In closing, we discuss implications these findings may have for clinical practice.
8:00 – 9:00 am | Location: Room 315
Ethical Challenges Facing Healthcare Workers in Settings of Extreme Violence
Matthew DeCamp, MD PhD; Grant Broussard, MSPH; Courtland Robinson, PhD; Leonard S. Rubenstein, JD
- Despite their protection under international law, attacks against health care facilities and workers occur with alarming frequency. During the war in Syria alone, more than 500 attacks have occurred against hospitals. The effects of these attacks devastatingly deprive access to health care for local populations, harm or kill health care workers, and disrupt core social institutions. Individuals and aid organizations working in these settings of extreme violence experience profoundly difficult choices, ranging from how to maintain an acceptable standard of care amidst chaos to whether to rebuild facilities in the same place (at risk of repeat attacks) or in a remote one (at risk of reducing accessibility to people in need). Here, we report findings from a multi-year project examining ethical challenges faced by health care workers and aid organizations operating in Syria. Through a systematic literature review, semi-structured interviews, and in-country workshops, our project described the full range of ethical challenges experienced in settings of extreme violence. These challenges were categorized according to eight core ethical obligations. Our analysis found areas of overlap, tension, and mutual reinforcement between the humanitarian principles to which humanitarian organizations are committed (i.e., neutrality, impartiality, humanity, and independence) and these ethical obligations. Our research suggests that, by incorporating ethical principles and frameworks for ethical decision-making, organizations operating in settings of extreme violence can find novel ways of fulfilling core humanitarian principles and managing the moral distress inherent in these settings. Five recommendations are proposed for how humanitarian organizations could operationalize ethical decision-making.
11:00 am – 12:00 pm | Location: Room 304-305
Global Health Justice and Governance
Anne Barnhill, PhD, Matthew McCoy, PhD, MA, MS, Jennifer Prah Ruger, PhD, MSc, MA, MSL, Eric Juengst, PhD, Danielle Wenner, PhD, Alex J. London, PhD

This panel will bring together four panelists around the common theme of global heath justice and governance comparing and contrasting perspectives from law and governance, political theory and public policy, global public health ethics and policy, and global health justice and governance, commenting on the recently published book from Oxford University Press on this topic. In a world beset by serious health disparities, by dangerous contagions that can circle the globe in hours, and by a confusion of health actors and systems, humankind needs a new vision, a new architecture, new coordination among renewed systems to ensure health for all. Global Health Justice and Governance lays out the critical problems facing the world today and offers a theory of justice and governance as a way to resolve these seemingly intractable issues. Panelists in this session will offer various perspectives on issues around this common theme of global health justice and governance, such as domestic and international health law and public health law, public preferences and debate about health, ethical issues related to resource allocation and policy, ethics of global public health and disease prevention in diverse societies, political theory and public and private institutions and organizations.
6:00 pm-8:00 pm | Location: Union Standard, 524 William Penn Place, Pittsburgh, PA
The Johns Hopkins Berman Institute and
the Wellcome Trust Reception
The Johns Hopkins Berman Institute of Bioethics and the Wellcome Trust invite you to a reception at the 2019 American Society for Bioethics + Humanities Meeting
–Saturday, October 26–
Concurrent Sessions – 10:45 – 11:45 am | Location: Room 309
Distrust Due to Injustice: How Should Health Pactitioners Respond?
Justin Bernstein, PhD, Joseph Ali, JD


Bi-directional trust is essential to the effective practice of medicine, research and public health globally. What influences individual and collective understanding and ability to maintain trust is interesting in its own right. In this panel, we wish to consider the moral and political significance of distrust in cases where patients and populations have been impacted by historical or ongoing abuses of trust. We will focus on two concrete cases to illustrate the nature of “distrust due to injustice” in public health and implications for response. The first case will illustrate the effect of distrust due to injustice on the collection and storage of health-related information to support development of population estimates of burdens of disease in low-resource countries. The second will reflect on vaccine hesitancy amongst some African Americans due to historical and ongoing betrayals of trust in the medical context. In such cases, we wish to consider not only what sorts of efforts ought to be made to mitigate the relevant form of distrust, but also what sorts of obligations of justice arise in light of this distrust, longer-term steps that ought to be undertaken to fulfill these obligations, as well as how these obligations should shape the relationship between patient and health worker, citizen, and state. We intend to incorporate perspectives from ethics, political philosophy, and public health in engaging with these questions.
1:15 pm-2:45 pm | Location: Room 306-307
Bioethics Book Club: Treating Pain During North America’s Opioid Epidemic
Travis N. Rieder, PhD, Anita Ho, PhD, MPH, Daniel Z. Buchman, PhD, MSW

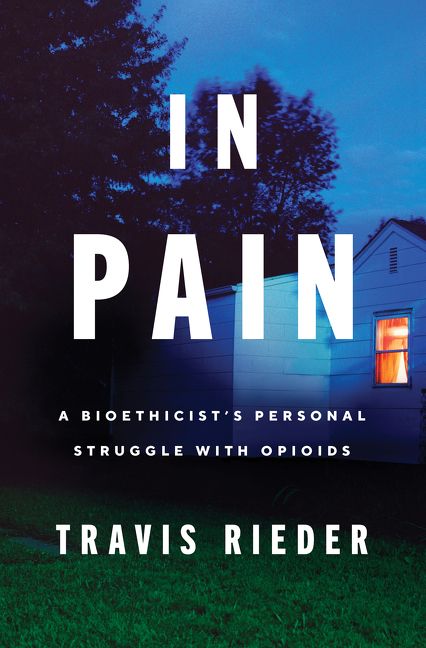
The goal of this panel is to bring a “book club” feel to ASBH, encouraging broad participation while ensuring rigorous scholarly commentary. The subject of the panel will be a new book (out summer 2019) on the ethics of opioid use in pain management against the backdrop of North America’s opioid crisis. The central question of the book is: what does responsible use of this medication look like, given its role in today’s opioid overdose crisis? Intended to reach a broader audience, the text is written by a bioethics scholar to bring crucial bioethics reasoning to the general public. The author (Panelist 1) will open the discussion with a 15-minute précis before turning it over to the other main discussants. They will then provide 15-minute commentaries on themes from the book, with Panelist 2 exploring the role that stigma plays in both pain and addiction medicine and Panelist 3 focusing on the use of shared decision making in contexts of uncertainty. To help promote audience engagement, we propose to use the ASBH listserve at the end of the summer to announce the Book Club and a call for short (5 minute), prepared commentaries on the book. With the remaining 40 minutes after the prepared portion of the panel, we will invite audience members selected from this call to deliver their prepared comments, which may include questions or challenges for any of the three panelists, after which we will take question from the rest of the audience.
1:15 pm-2:45 pm | Location: Room 316

Addressing health disparities is a policy priority in the United States. In addition to prioritizing disparities between gender, racial, and ethnic groups, U.S. policymakers and researchers also prioritize disparities related to disability status. Although great efforts have been directed towards a better understanding of health disparities over the past several decades, some have lamented that this progress has been slowed by the lack of shared conceptual terminology. The attempt to standardize health disparities research terminology, however, is complicated by the normative assumptions underpinning and motivating all efforts to measure and address health disparities. This presentation will consider the unique ways these complications manifest in the context of disability-related disparities. After introducing a distinction between health differences, health disparities, and health inequities, it will describe some of the ethical justifications for caring about health disparities in the first place. Disability status is a morally suspect class in the context of American society and history. Thus, it warrants attention from health disparities researchers. Yet, the complicated relationship between disability and health raises unique difficulties for the measurement of disability-related health disparities. These difficulties are further complicated by the lack of consensus over what justice requires us to provide to people with disabilities. As research increasingly focuses on disability-related disparities, these difficulties will need to be acknowledged and addressed.
1:15 pm–2:45 pm | Location: Room 302
Hyde and Go Seek Funding: Resource Allocation by Grassroots Abortion Funds
Ariella Messing, PhD Candidate

Abortion is the only medical procedure that the federal government is prohibited from funding and that the Affordable Care Act explicitly permits states to ban health insurers from covering. The compounded effects of federal and state policies restricting insurance coverage of abortion and regulating the provision of abortion care have created significant financial obstacles to the constitutionally protected right to abortion; low-income women are often unable to access abortion care. In response, communities have created abortion funds, locally-run grassroots organizations that provide financial and logistical assistance to people who need help accessing abortion care. Over 70 autonomous funds have developed organically in response to their local environments; while all funds may share the same goals, their priorities and approaches often differ. This exploratory study describes the variation in abortion funds and examines the ethical values and principles that drive organizational decisions. Data was collected using in-depth semi-structured interviews with a purposive sample of 33 abortion fund volunteers and staff at 26 abortions funds across the United States. Topics covered in the interviews include the fundraising process, the values that guide fund allocation decision-making in the context of scarcity, and case management structures, among other process and organizational decisions and rationales. This presentation examines the themes that arose across funds in different geographical and political contexts and the ethical implications of relying on volunteer-based grassroots funding for the provision of a basic health care service.
1:15 pm–2:45 pm | Location: Room 302 (Same session as directly above)
Reproductive Injustice at the Border
Ariella Messing, PhD Candidate, Rachel E. Fabi, PhD; Joanne Rosen, JD

Recent news reports from the U.S.-Mexico border have detailed alarming stories of public health and ethical violations by the current administration: the deaths of immigrant children in U.S. custody; unaccompanied minors prevented from accessing legal and safe abortions; stillbirths among pregnant detainees; infants torn from their mothers by Customs and Border Protection agents. These stories are often reported in isolation, painting a picture of individual incidents of abuse, or of standalone policies. In this presentation, we examine the recent changes in immigration policies that have systematized this mistreatment, including restrictions on abortion access, unsafe treatment of pregnant immigrants, and the separation of families in immigration detention. When considered through a traditional reproductive rights framework, the Trump administration’s “pro-life” or “pro-family” approach to undocumented minors who seek to terminate their pregnancies may seem at odds with attempts to deny appropriate prenatal care to undocumented adults who wish to continue their pregnancies or with the practice of separating families at the border.
In this presentation, we introduce the Reproductive Justice framework and then demonstrate how these policies and practices violate all three primary tenets of Reproductive Justice: the right to have children, the right not have children, and the right to parent children in safe and secure environments. We argue that when analyzed within this conceptual framework, these policies can be seen as components of a single, targeted strategy to control the reproductive autonomy of vulnerable immigrants.
3:00 pm- 4:00 pm | Location: West Atrium
Against Principled Thresholds: A Conventionalist Defense of Abortion

There is a moral presumption against killing an entity with full moral status (FMS). Those opposed to abortion often object that defenses of the moral permissibility of abortion cannot identify a principled threshold at which point fetuses acquire FMS. While some attempt to avoid this conclusion or even bite bullets in response, I offer a different reply: defenders of the moral permissibility of abortion should embrace the claim that there isn’t a principled threshold for FMS. My argument for this claim turns on the observation that in some contexts, the difficulty in identifying principled thresholds for some to have rights against others is evidence that, at the margins, there are no principled thresholds for the possession of these rights. Instead, such thresholds have to be established conventionally or through law. I illustrate this point by considering difficulties in identifying thresholds for property rights, difficulties that count in favor of the claim that boundaries of property rights have to be defined conventionally or legally. Defenders of the moral permissibility of abortion should take a similar tack. Questions about when some entity acquires FMS is a question about boundaries, albeit concerning rights that accompany FMS rather than rights that accompany ownership. The difficulty in identifying boundaries for FMS is evidence that there is no principled threshold for FMS. Instead, the boundaries for FMS have to be established conventionally or legally. Accordingly, it is unconvincing abortion is impermissible on the grounds that liberals cannot identify a principled threshold for full moral status.
4:15 pm-5:45 pm | Location: Room 304-305
Making Decisions with Parents about Chronic Mechanical Ventilation for their Children: Are We Helping or Harming the Dialogue?
Nicholas A. Jabre, MD, MS; Benjamin Wilfond, MD; Laura Sterni, MD; Renee Boss, MD, MHS


The decision to initiate or forgo chronic mechanical ventilation in a child with prolonged respiratory failure is complex and profound. Clinicians and bioethicists may struggle to weigh the implications of each choice, especially when death is a possible outcome. Guidance toward initiating chronic mechanical ventilation places families without adequate supports at risk of financial strain, social isolation, or psychological distress. Alternatively, guidance toward withholding ventilation risks alienating families who are singularly focused on their child’s survival. Deepening our understanding of how parents perceive interactions with clinicians while deliberating chronic mechanical ventilation could help us engage them in a more personalized manner that better addresses their individual goals. We conducted a multi-center, qualitative study examining parents’ experiences of decision-making surrounding chronic mechanical ventilation. We interviewed 40 parents across three regions in the United States from a variety of socioeconomic and familial backgrounds who made a decision to either initiate or forgo chronic mechanical ventilation for their child within the past three years. Here, we report the experiences of those parents and whether their interactions with clinicians during the deliberation process were perceived as helpful or harmful. Preliminary results show that parents’ individual values and viewpoints regarding life with mechanical ventilation heavily shape their approach to this high-stakes decision. Healthcare professionals should practice intentional curiosity about the unique attitudes and perspectives of parents in order to provide quality guidance that is both patient and family-centered.
–Sunday, October 27–
Concurrent Sessions – 8:00 am-9:00 am | Location: Room 310-311
The Ethical, Legal, and Social Implications of Vaccinomics in the United States
Jennifer E. Gerber, MSc; Janesse Brewer, MPA; Andrea Sutherland, MD, MSc, MPH; Rupali J. Limaye, PhD, MPH, MA; Gail Geller, ScD, MHS; Jeff P. Kahn, PhD, MPH; Daniel A. Salmon, PhD, MPH


objectives: Vaccinomics may use genomics to make vaccines safer and more effective, increasing resilience to vaccine preventable infections. Public values around the ethical, legal, and social implications (ELSI) of vaccinomics were explored. methods: Adults ≥18 years-old attended discussion groups in Boulder, CO and Baltimore, MD in 2018. 95 participants (64% female) were recruited through community organizations and schools, approximating the sociodemographic distribution of each city. After a short animation introduced vaccinomics, participants were randomly assigned to 1 of 7 nested discussion groups. results: Participants generally supported the use of genomics to enhance the safety and effectiveness of vaccines. Ethical issues regarding vaccinomics included privacy/confidentiality, discrimination based on genetic information, prevention of adverse reactions, and justice. Vaccinomics-related ELSI concerns varied by age and trust in industry, government, medicine, and science. Fear of increased health insurance rates or losing coverage due to genetic information discovered through vaccinomics was higher among older versus younger participants. Participants trust government to implement vaccinomics more than industry. Participants who experienced or witnessed an adverse event following immunization (“remembrance”) expressed greater interest in vaccinomics’ potential to personalize vaccines. Participants in both cities recalled historical cases of African Americans’ rights and medical research ethics being violated. They worried vaccinomics would not be applied in ways that benefit vulnerable populations, contributing to stigmatization of marginalized communities. conclusion: These findings are informing the development of a nationwide online survey of vaccinomics-related ELSI concerns and support for personalized vaccines and schedules, overall and by level of vaccine confidence, among U.S. adults.
11:00 am-12:30 pm | Location: Room 320
Disrespectful Language in Prenatal Records
Marielle S. Gross, MD, MBE; Mary Catherine Beach, MD, MPH


Language within medical records may reflect clinicians’ biases and convey stigma about patients from one clinician to another. Women may be especially vulnerable to biases and judgment from clinicians during pregnancy, a time of frequent healthcare engagement about morally-fraught reproductive health. We conducted qualitative linguistic analysis of the history and physical (H&P) from 100 randomly selected women admitted for delivery at our academic center in 2017 to characterize language in prenatal records that may convey disrespect for pregnant women.
With thematic analysis, we identified three types of disrespect: objectifying women’s bodies, testimonial injustice, and signaling the “bad mother.” Women’s bodies are objectified by gratuitous, inappropriately intimate details (‘multiple gushes soaking her underwear and trickling down her leg’). Testimonial injustice occurs when subjective experiences, especially of pain, are trivialized and discredited by juxtaposing patient testimony with “objective data” (‘patient reports unbearable contractions, but cervix remains unchanged.’) Finally, clinicians evoke the “bad mother” by highlighting nonadherence (‘only seen in clinic once’ or ‘but declines genetic screening’), questioning judgment (‘aware of⋯increased risk of maternal and fetal morbidity and mortality, still desires trial of labor’), and implying poor self-care (‘patient has no idea when last pap smear was done’).
Prenatal records manifest disrespect for, and often insidiously mock, pregnant women. We discuss textual cues that may help identify disrespectful language, and potential strategies for preventing healthcare providers from codifying and propagating prejudice.
Seminar Series
Mario Macis, PhD
- National Institutes of Health (NIH) “Creative and Novel Ideas in HIV Research (CNIHR) grant for “Behavioral nudges, information and incentives for HIV testing: A field experiment in Ecuador”, 2016-18.
- Johns Hopkins University Discovery Award, 2016.
- Johns Hopkins University early-career Catalyst Award, 2015.
- Johns Hopkins University Alumni Association Excellence in Teaching Award, 2013.
- National Science Foundation (NSF) Grant for “Field Experiments on Incentives and Blood Donations”, 2009-12.
Berman Featured at “Hopkins on the Hill”
To underscore the role and subsequent results of federally-funded research, Johns Hopkins hosted a showcase of 21 project teams from all corners of the institution, including three Berman Institute faculty, at a special June 12, event in the House of Representatives, called Hopkins on the Hill.
Berman Institute Associate Director for Global Programs Joe Ali was selected to present the Berman Institute’s training programs for scholars in sub-Saharan Africa.
“Debates about ethical controversies in global health research are often dominated by voices from the global ‘North,’” said Ali. “Federally-funded global bioethics initiatives empower sub-Saharan African researchers and institutions to meaningfully engage in local and international research and deliberations about the ethics of such research.”
Ali was joined by Berman Institute associate faculty member Megan Collins, whose presentation was titled “A Vision for Success: How Providing Glasses is Helping Baltimore’s Youth.”
Also presenting was Carey Business School professor Mario Macis, who recently became an affiliate member of the Berman Institute faculty. Macis presented about “Motivating HIV Testing with Incentives and Behavioral Nudges.”
“We are thrilled to highlight these early career researchers whose scientific investigations and innovations represent a fraction of the remarkable, publicly funded research underway at Johns Hopkins,” says JHU President Ronald J. Daniels. “Their work is not only advancing scientific understanding, but also creating products and therapies that improve the quality of life in America.”
Daniels has long been an advocate for the importance of federal support for research, especially for young researchers. Johns Hopkins has led U.S. universities in research and development spending for 39 consecutive years, putting a record $2.562 billion in FY2017 into projects to cure disease, promote human health, advance technology, and expand knowledge of the universe and ourselves.
“The wide breadth of research at Johns Hopkins, from engineering to the life sciences, from the social sciences to the humanities, continues to be funded at record levels,” says Denis Wirtz, the university’s vice provost for research. “This support allows the institution to uphold its critical mission of fostering independent and original research, and bringing the benefits of discovery to the world.”
Berman Institute Launches SNF Bioethics Academy
The Johns Hopkins Berman Institute of Bioethics (JHU) in conjunction with the Bioethics Chair at the Swiss Federal Institute of Technology (ETH) have launched a new initiative called the Stavros Niarchos Foundation Bioethics Academy (SNFBA). The SNFBA is exclusively supported by the Stavros Niarchos Foundation (SNF) and was created with the intent to support and enhance knowledge and awareness for bioethics in Greece.
Visit the SNF Bioethics Academy for full information.
 The three main components of the SNFBA are:
The three main components of the SNFBA are:
- An intensive bioethics summer course offered every June, beginning in 2019, in Athens, Greece;
- Annual in-depth workshops alternating between Zurich, Switzerland (hosted at ETH) and Baltimore, USA (hosted by JHU), beginning winter 2021;
- An alumni network that provides ongoing connections with other Greek bioethics professionals, resources and information through a dedicated website, and virtual discussions via webinar.
Summer Bioethics Course
June 20-22, 2019
Stavros Niarchos Foundation Cultural Center
The SNFBA is co-directed by Prof. Jeffrey Kahn, the Andreas C. Dracopoulos Director of the Johns Hopkins Berman Institute of Bioethics (JHU), and Prof. Effy Vayena, Head of the Health Ethics and Policy Lab at the Swiss Federal Institute of Technology in Zurich (ETH).
The inaugural Bioethics Summer Course in 2019 is a three-day course including lectures by international faculty followed by small group discussions facilitated by JHU and ETH faculty and Greek bioethics experts.
IN-DEPTH WINTER TWO-DAY WORKSHOPS
These workshops will alternate between Zurich, Switzerland (hosted at ETH) and Baltimore, U.S.A. (hosted at JHU) and will include faculty from the Summer Course along with additional visiting faculty. Approximately 20 attendees will be invited per workshop, based on their interest in further training and education in bioethics and their aptitude for bioethics.
Workshop content will be topical and developed with input from the selected participants. The program will include presentations by all participants, intensive case analysis and consultation (with at least some actual cases provided by participants), train-the-trainer exercises so that participants can return to their institutions/workplaces to help educate their peers, and additional specialized content.
ALUMNI NETWORK
The third component of the Stavros Niarchos Foundation Bioethics Academy will be an Alumni Network created for summer course participants, all of whom will automatically be members.
In addition to providing news, resources and information via a dedicated SNFBA website, email, and social media channels, the network will be a means for staying in touch with other SNFBA alumni in Greece and bioethics faculty at JHU and ETH. The network will host virtual discussions via webinar and convene in-person reunions and events in conjunction with the timing of the annual summer course and SNF Annual International Conference in Athens.
“Containment” Explores Infectious Disease Response
Led by BRIDGES team members Graham Mooney and Rebecca Wilbanks, the Berman Institute of Bioethics convened the Robert H. Levi Symposium, “Containment: Exploring the History, Politics, and Ethics of Infectious Disease Response in a Post-Genomic World” on March 11-12.
Visit the Symposium website.
The symposium kicked off with a public event featuring remarks by Kaci Hickox and Gregg Mitman. Hickox graduated from the Johns Hopkins School of Nursing and now works for Doctors Without Borders as an infection prevention and control advisor. She spoke of her experiences treating Ebola patients in West Africa and her decision to mount a legal challenge to the quarantine order that was imposed on her when she returned to the US.
Mitman is a historian at the University of Wisconsin-Madison and the director of In the Shadow of Ebola, which was screened at the public event. The film follows a family affected by the 2014 Ebola outbreak in Liberia. Both Mitman and Hickox highlighted the way in which politicized responses to contagious diseases can compound the harms suffered by affected communities. After the film screening Berman Institute faculty member Jeremy Greene, the chair of the History of Medicine Department, moderated a discussion that included questions from audience members.
The following day, a broadly interdisciplinary group of researchers met at the Berman Institute to develop a research agenda on the social and ethical dimensions of infectious disease response. The working group brought together scholars from across the university, including the School of Medicine, the Center for Health Security, the Berman Institute of Bioethics, and the Krieger School of Arts and Sciences, as well as external experts from anthropology, sociology, literature, law, and philosophy. Topics discussed included the ongoing Ebola outbreak in the Democratic Republic of Congo, where treatment facilities and medical providers have recently been under attack. These events underscore the need for culturally and historically informed approaches to providing care. Workshop participants will collaborate to disseminate the insights and knowledge generated by the workshop in peer-reviewed publications.