For comprehensive Covid-19 Ethics and Policy Resources, visit our dedicated webpage, bioethics.jhu.edu/coronavirus.
The ongoing coronavirus outbreak vividly demonstrates the important role of bioethicists in leading the charge for equitable and effective public health policies.
“Through years of experience and scholarship, and tested through multiple threatened and actual epidemics, there now exists a rough consensus about the ethical principles that should guide responses to this latest threat,” said Jeffrey Kahn, Andreas C. Dracopoulos Director of the Berman Institute of Bioethics. “Bioethicists from the Berman Institute have been leaders in shaping this framework.”
The Berman Institute is working to disseminate these ideas through social media, appearances in traditional news media, and through other means, as widely as possible on an ever-expanding range of issues, including:
Human Research
“For reasons of safety, efficacy, and ethics, it’s usually better to test vaccines on animals before humans. You have to have good reason to say, ‘We need to go straight to humans or go to humans at this particular point.'”
“Kahn worries about people signing up to be in the trial because they think the vaccine could give them immunity before it becomes available to everyone else. In reality, this kind of early trial is just to make sure that the vaccine is not toxic and does indeed provoke some kind of immune response in people. Participants are very unlikely to be fully immunized to the virus over the course of their participation.”
Travel Restrictions
“A critical principle in outbreak response is that governments should implement the least restrictive measure that can still achieve the public health objective. The goal is to balance the freedom of individuals against the restrictions on freedom required to achieve legitimate protections of the public’s health, with public and transparent justification of policy decisions. Quarantine is considered a measure of last resort given the severe restrictions it imposes on individual liberty.”
Inequitable Impact of School Closings
“As in all public health emergencies, poor children and poor families will suffer the most. An ethically defensible policy of school closures needs not only to meet the bar of public health necessity. Government agencies and community organizations in education, nutrition assistance and housing, as well as public health, must also be planning to take active measures to mitigate the disproportionate burden that will fall on our most vulnerable children.”
Dr. Faden’s prescient Education Week piece helped prompt discussion among K-12 educators nationwide. Officials in numerous states have sought USDA waivers that will enable them to continue providing free meals during school closures.
Allocation of Scarce Resources
“It is appropriate and accurate to reassure the public that most people who contract Covid-19 will recover fully on their own. At the same time, the public needs to be prepared for the possibility of more dire scenarios. Participants in our study were adamant that politicians, and health officials, be transparent and honest about the prospect of and plans for the rationing of ventilators and other equipment. In health emergencies, experts often ask the public to heed the advice of public health professionals; in the case of planning for situations involving scarcity, it is equally important that the experts heed the advice of the public.”
Inequitable Impact of Social Distancing
“The implications of some of these public health measures are so wildly different for people who are differently situated in the United States that the social distancing [decision] is not our only decision. It’s our first one, and then there’s a very different set of ethical dominos that follow from that.”
Kass listed a number of ethical considerations she’s concerned about, like making sure there’s adequate income replacement for workers unable to earn a living, making sure grocery stores stay open and accessible, and even making sure people have access to the creature comforts that make social distancing bearable.
Inequity of Work Requirements During Pandemic
“Income replacement for people whose employment has been curtailed by the government isn’t just an economic issue, it’s an ethical one. Likewise, we need to consider what to do for workers in jobs where sufficient protection from infection cannot be provided. While we have expectations of certain healthcare professionals, like doctors and nurses, who have taken oaths to continue working even when it puts them at personal risk, the same isn’t true for hospital support staff or grocery store checkers. We can’t simply expect those workers to continue facing risks that others can avoid.”
Equity in Vaccine Development
“Historically, the interests of pregnant women have not been adequately included in global responses to outbreaks and epidemics. As the world rushes to develop new vaccines against Covid-19, we must ensure that, this time, pregnant women and their babies will not be left behind. Developing a coronavirus vaccine that they are unable to use would be not only a tragedy but a grave injustice.
The article was included as required reading for the 38th Annual Congressional Leadership Conference of the American College of Obstetricians and Gynecologists, as physicians came to Washington from across the country to meet legislators and help shape public policy. Faden and Krubiner’s co-author of the STAT and Boston Globe article and collaborator in the PREVENT project, Ruth Karron of the Johns Hopkins Vaccine Initiative, was quoted in a March 3 New York Times article, “What Pregnant Women Should Know About Coronavirus.”
Patient Privacy and Contact Tracing
“Doctors don’t out people. Whether it’s HIV, syphilis, coronavirus or anything else, people simply won’t show up to their doctor if they feel they might be outed for a condition.”
Impact on Incarcerated Individuals
Detention and correctional spaces are the “perfect environment for the spread of COVID-19. So when we talk about social distancing, it’s almost impossible in prisons unless you have complete lockdown – basically, put everybody in solitary confinement.”
The Berman Institute continue to offer insights and expertise to aid in the response to the monumental challenges posed by the outbreak.
Related Berman Institute Resources
- 2019 Robert H. Levi Symposium: “Containment: Exploring the History, Politics and Ethics of Infectious Disease Response in a Post-Genomic World”
This symposium brought together experts to explore the shifting politics of containment from the nineteenth century through the Cold War to the present, to inform best practices for infectious disease preparedness and response from the local to the global scale.
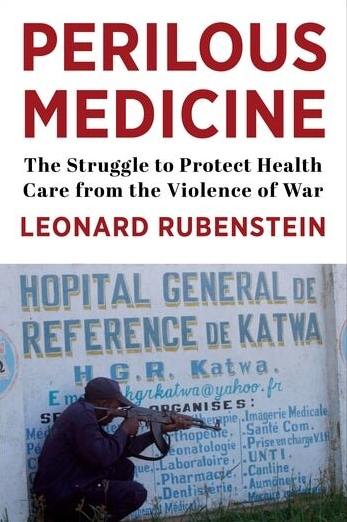
- Ethics Guidance for the Public Health Containment of Serious Infectious Disease Outbreaks in Low Income Settings: Lessons from Ebola
In 2019, the Berman Institute and partners published a report and other resources, as products from a project to provide an ethics guidance document for public health professionals to use in infectious disease outbreak response. The guidance makes clear that regardless of geography, infectious disease outbreak response strategies should be effective, fair, respectful and transparent.
- The Bellagio Meeting on Social Justice and Influenza
In 2006, Dr. Faden was among a group of 24 experts in public health, animal health, virology, medicine, public policy, bioethics, law and human rights from 11 countries that met to consider questions of social justice and the threat of avian and human pandemic influenza. The consensus of the group was that efforts to prepare for and respond to a pandemic should take account of the needs and interests of the disadvantaged.