2022 SNFBA Course Materials
Sunday, 19 June
14:00-14:15 Welcome
- Jeffrey Kahn, PhD, MPH
Andreas C. Dracopoulos Director of the Johns Hopkins Berman Institute of Bioethics
Robert Henry Levi and Ryda Hecht Levi Professor of Bioethics and Public Policy - Effy Vayena, PhD
Chair in Bioethics, ETH Zurich
Chair of the Hellenic National Bioethics and Technoethics Commission
14:15-15:15 Introduction of Faculty and Participants
15:15-16:15 Session I: Foundational Principles in the Ethics of Research Involving Human Participants (Remote Presentation)
- Tom Beauchamp, PhD
Professor Emeritus, Georgetown University
16:15-16:45 Break
16:45-17:45 Session 2: Overview of Ethics of Research with Human Subjects and Lessons from the Pandemic (Remote Presentation)
- Ruth Faden, PhD, MPH
Founder, Johns Hopkins Berman Institute of Bioethics
Philip Franklin Wagley Professor of Biomedical Ethics
17:45-18:30 Small Group Session (Case #1 Discussion)
18:30- Cocktail Reception and Dinner
Monday, 20 June
08:30-09:00 Coffee
09:00-10:15 Session 3: Ethics in the Design and Implementation of Clinical Research
- Jeremy Sugarman, MD, MPH, MA
Deputy Director for Medicine, Johns Hopkins Berman Institute of Bioethics
Harvey M. Meyerhoff Professor of Bioethics and Medicine
10:15-11:00 Session 4: Informed Consent in Practice
- Jeremy Sugarman, MD, MPH, MA
Deputy Director for Medicine, Johns Hopkins Berman Institute of Bioethics
Harvey M. Meyerhoff Professor of Bioethics and Medicine
11:00-11:30 Break
11:30-12:30 Small Group Session (Case #2 Discussion)
12:30-14:00 Lunch
14:00-15:00 Session 5: Ethics and Genetic Research
- Effy Vayena, PhD
Professor and Chair in Bioethics, ETH Zurich
Chair of the Hellenic National Bioethics and Technoethics Commission
15:00-16:00 Session 6: Ethics and Digital Health Research
- Alessandro Blasimme, PhD
Senior Scientist, Chair in Bioethics, ETH Zurich
16:00-17:00 Small Group Session (Case #3 Discussion)
17:00-18:00 Free Time
18:00- Dinner
Tuesday, 21 June
08:30-09:00 Coffee
09:00-10:00 Ethics and Public Health Research
- Jeffrey Kahn, PhD, MPH
Andreas C. Dracopoulos Director of the Johns Hopkins Berman Institute of Bioethics
Robert Henry Levi and Ryda Hecht Levi Professor of Bioethics and Public Policy
10:00-11:00 Session 8: Lightning Talks (4 x 15 minutes)
- Effy Vayena: Ethical Issues in De-Centralised Clinical Trials
- Alessandro Blasimme: Ethical Issues in AI Research: The Case of ADHD
- Jeffrey Kahn: Ethics and Human Challenges Studies
- Jeremy Sugarman: New Ethics Guidance for Human Stem Cell Research
11:00-11:30 Break
11:30-12:30 Small Group Session (Case #4 Discussion)
12:30-14:00 Lunch
14:00-14:30 Wrap-up and Certificates of Completion
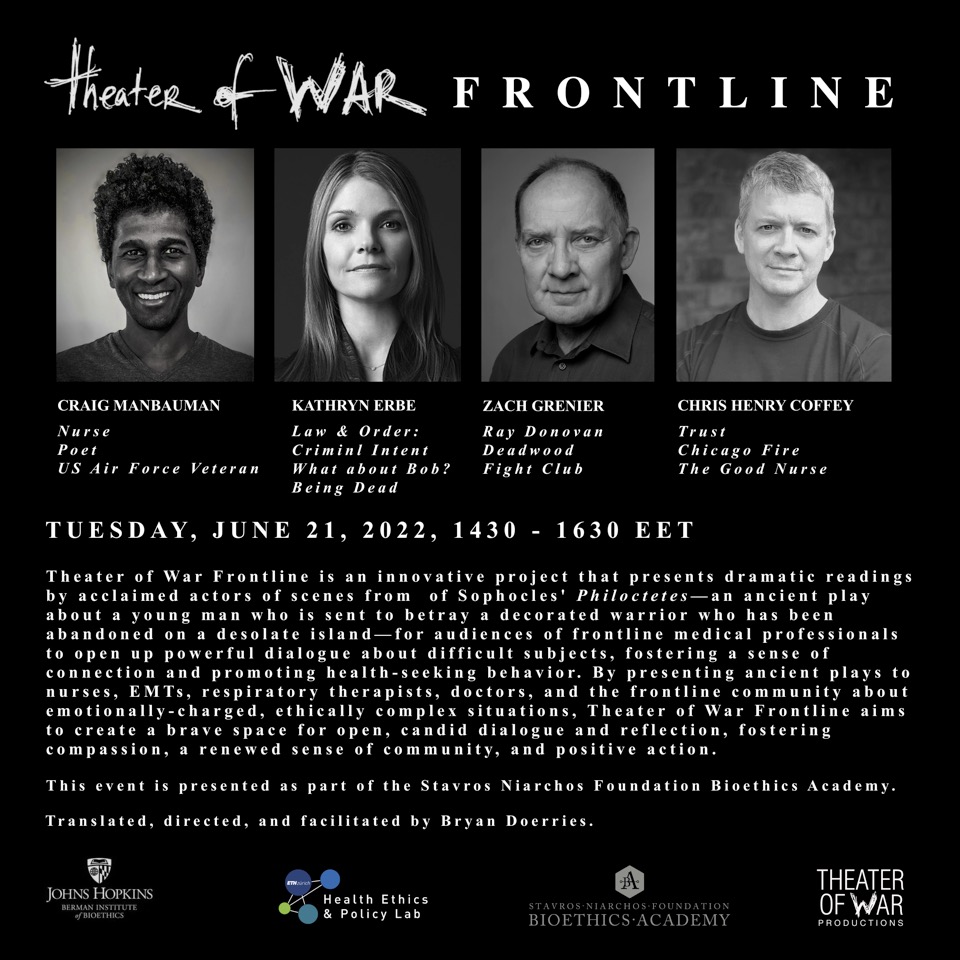
14:30-16:30 Theater of War Performance and Discussion
16:45-19:00 Alumni Welcome & Networking
— 16:45-17:05 Speed Dating
— 17:05-17:25 Alumni Updates Panel
— 17:25-17:45 Greek National Bioethics/Technoethics Commission Update
- Effy Vayena, PhD
Professor and Chair in Bioethics, ETH Zurich
Chair of the Hellenic National Bioethics and Technoethics Commission - Charalambos Tsekeris
Vice Chair, National Commission for Bioethics & Technoethics; Res Assoc Professor, National Centre for Social Research, Greece
17:45-17:50 Alumni Workshops in the United States & Switzerland
- Jeffrey Kahn, PhD, MPH
Andreas C. Dracopoulos Director of the Johns Hopkins Berman Institute of Bioethics
Robert Henry Levi and Ryda Hecht Levi Professor of Bioethics and Public Policy